
Sudden cardiac death in young athletes

High school basketball requires skill and rigorous training. In rare but highly publicized cases, it can also bring cardiac issues to the surface. (U.S. Army photo by Chuck Gannon)
In January, a student athlete at Spartanburg High School in South Carolina collapsed after a basketball game against rival Riverside. Two coaches performed CPR and used a defibrillator until paramedics arrived. The teenager survived. Less than a month earlier at John Bowne High School in Flushing, Queens, New York, a student athlete, who his mother described as “healthy as you could imagine” collapsed during basketball practice. Sadly, coaches were unable to revive him. It was later determined Lenny Pierre, the New York student, had a major blood vessel in his heart that was in an abnormal location, resulting in sudden cardiac arrest. He was only 16.
Sudden cardiac events can occur in seemingly healthy young people in their teens or twenties, including young servicemembers. “Being in the military, you are signing yourself up for an active lifestyle, and I think most people want that,” said Army Lt. Col. Erik Johnson, a pediatric cardiologist at Walter Reed National Military Medical Center in Bethesda, Maryland. “I think that’s encouraged in dependents as well. Any accurate information is helpful in making sure families know what to look for in their kids so they get them to appropriate providers if necessary.”
Johnson said there are several possible causes of sudden cardiac death in young competitive athletes, such as hypertrophic cardiomyopathy or HCM. “It is actually fairly common in the general population,” said Johnson. “About 1 in 500 people have this, and it accounts for about a third of sudden cardiac death in young athletes.”
While HCM is hereditary, other cardiac conditions are not, such as the coronary artery abnormality that caused Lenny Pierre’s death. “A coronary artery that doesn’t come off where it normally should causes another 15 to 20 percent of sudden cardiac death,” said Johnson. “Overall, more than 50 percent of the cases of sudden cardiac death in young athletes are caused by either HCM or coronary artery abnormalities.”
Heart problems in young people often go undetected, leaving providers to look for clues. “A provider could look at a child and suspect Marfan syndrome,” said Johnson. According to the National Institutes of Health, Marfan syndrome is a disorder that affects the connective tissue and may result in abnormalities such as dilation and rupture of the aorta, a catastrophic and often fatal event. Johnson added that a diagnosis of Marfan syndrome would mean exercise restrictions for the child.
Other causes of sudden cardiac issues in athletes include arrhythmias, myocarditis, and congenital heart disease. Arrhythmias are irregular heartbeats (too fast or too slow) which could be genetic or the result of a direct blow to the chest by a batted ball or an on-field collision. Myocarditis is an infection of the muscle of the heart that affects the heart’s ability to pump well. Congenital heart disease encompasses a number of structural problems of the heart that a child may be born with.
Johnson urges parents of young athletes and their coaches to be aware of signs and symptoms that indicate the need to see a provider before a catastrophic event. These include:
- Chest pain with exertion every time a child tries to run or participate in some other kind of aerobic activity
- Irregular heartbeat, where a child complains that the heart is beating too fast or too slow, or is skipping beats
- Loss of consciousness during exercise
- Decreased exercise tolerance, where a child feels fatigued with a level of exercise that was previously routine
“The American Heart Association and the American College of Cardiology have put out guidelines looking at sports participation in patients who have [diagnosed] cardiac disease,” said Johnson. The guidelines, updated in 2015, list recommendations and restrictions for competitive athletes who engage in “vigorous training” while living with 15 different classifications of heart conditions.
While this information may be alarming, parents just need to be vigilant. Cases of sudden cardiac death in young athletes are exceedingly rare, with about 1 occurrence in 80,000 – 100,000 children per year, according to Johnson. In an otherwise healthy child, there is no need to place restrictions on activities or sports due to the remote possibility that something bad could happen.
There is clear evidence that activity like sports participation improves both the physical and mental health of children. “Some of the best screening we can do is to ask, ‘do they have symptoms?’ said Johnson. “The answers can clue you into looking deeper into some of these uncommon things.” Uncommon things that could save a life.
Too much pressure: Hypertension a leading cause of heart disease
Article
3/5/2019
Healthy lifestyle now can help prevent disorder later
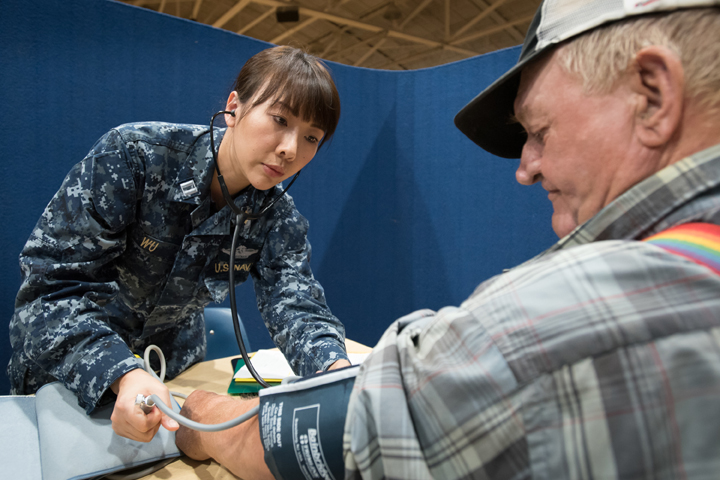
Military health leaders take part in inaugural American Red Cross Advanced Life Support class
Article
3/4/2019
The transition to the American Red Cross Resuscitation Suite officially began October 1, 2018
Malaria
Infographic
3/1/2019

Since 1999, the Medical Surveillance Monthly Report has published regular updates on the incidence of malaria among U.S. service members. The MSMR’s focus on malaria reflects both historical lessons learned about this mosquito-borne disease and the continuing threat that it poses to military operations and service members’ health.
Glaucoma
Infographic
3/1/2019

This report describes an analysis using the Defense Medical Surveillance System to identify all active component service members with an incident diagnosis of glaucoma during the period between 2013 and 2017.
Adenovirus
Infographic
3/1/2019

During August–September 2016, U.S. Naval Academy clinical staff noted an increase in students presenting with acute respiratory illness (ARI). An investigation was conducted to determine the extent and cause of the outbreak.
Air Force units partner for aeromedical evacuation exercise
Article
2/27/2019

With a critical care mission spanning half the globe, practicing is vital to patient survivability
The eyes have it: Seven tips for maintaining vision
Article
2/25/2019

Most eye injuries are preventable, experts say
Focus on heart-healthy diet is perfect fit for February
Article
2/22/2019

With the typical American diet and lifestyle, many people put themselves at risk for developing various heart diseases
Military health care transitions to new life support training provider
Article
2/20/2019

American Red Cross courses better suited to military needs
Taking care of your heart with TRICARE benefits
Article
2/19/2019

Getting preventive screenings now could save your life tomorrow
The simple – and complicated – task of shoveling snow
Article
2/5/2019

When in the throes of winter weather, there are ways to prepare for a successful, injury-free snow shoveling activity
Stroke prevention awareness
Article
2/4/2019
Stroke is the fifth leading cause of death in the U.S.
MSMR Vol. 26 No. 2 - February 2019
Report
2/1/2019
A monthly publication of the Armed Forces Health Surveillance Branch. This issue of the peer-reviewed journal contains the following articles: Non-alcoholic fatty liver disease (NAFLD), active component, U.S. Armed Forces, 2000–2017; Cardiovascular disease-related medical evacuations, active and reserve components, U.S. Armed Forces, 1 October 2001– ...
Army Medicine joins forces with civilian hospitals to sustain medical readiness
Article
1/31/2019

The AMCT3 program addresses the 2017 NDAA directive for the Military Health System to establish partnerships to maintain trauma care competency
Acute Flaccid Myelitis Case Reporting
Infographic
1/29/2019

This case highlights important clinical characteristics of acute flaccid myelitis and emphasizes the importance of including AFM in the differential diagnosis when evaluating active duty service members and Military Health System beneficiaries presenting with paralysis.
No comments:
Post a Comment