
Atezolizumab Approved for Some Patients with Triple-Negative Breast Cancer
March 28, 2019, by NCI Staff
On March 8, the Food and Drug Administration (FDA) granted an accelerated approval for the immunotherapy drug atezolizumab (Tecentriq) in combination with chemotherapy for the initial treatment of some women with advanced triple-negative breast cancer.
The combination therapy is the first FDA-approved regimen for breast cancer to include immunotherapy. Accelerated approvals are based on early data from studies which strongly suggest that patients benefit from a treatment. Under accelerated approvals, FDA requires the drug manufacturer to conduct additional studies to confirm that the therapy has a clinical benefit.
The approval is for atezolizumab used in combination with the chemotherapy drug nab–paclitaxel (Abraxane). The combination is approved for women with locally advanced or metastatictriple-negative breast cancer that cannot be treated surgically and whose tumors are positive for a protein called PD-L1.
FDA also approved a companion diagnostic test called the VENTANA PD-L1 (SP142) Assay, which must be used to identify patients with triple-negative breast cancer who are candidates for treatment with this immunotherapy–chemotherapy combination.
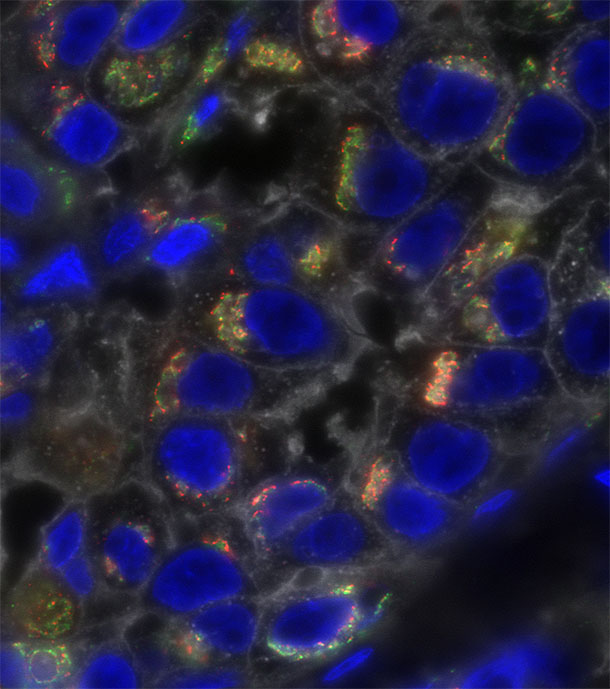
Atezolizumab belongs to a class of drugs known as immune checkpoint inhibitors. By inhibiting immune checkpoint proteins such as PD-L1 or PD-1, these drugs “release the brakes” on the immune system, enhancing the ability of immune cells to find and attack cancer cells.
Clinical Trial Results
FDA’s approval was based on results from the phase 3 IMpassion130 clinical trial, which compared atezolizumab plus nab-paclitaxel with placebo plus nab-paclitaxel as the initial, or first-line, treatment for patients with triple-negative breast cancer.
The trial included 902 patients with locally advanced or metastatic triple-negative breast cancer who had not received prior chemotherapy or targeted therapy for metastatic disease.
Among the 369 patients in the trial with PD-L1–positive tumors, the median progression-free survival was 7.4 months for patients treated with atezolizumab plus chemotherapy and 4.8 months for those who received placebo plus chemotherapy.
The objective response rate was 53% in the atezolizumab group versus 33% for the placebo group.
“It was very clear from the trial results that the patients who benefited from the combination therapy were those with PD-L1–positive tumors,” said Leisha A. Emens, M.D., Ph.D., of the University of Pittsburgh Medical Center Hillman Cancer Center and Magee Women's Hospital, one of the trial’s lead investigators.
In triple-negative breast cancer, PD-L1 is expressed mainly on immune cells that infiltrate tumors, Dr. Emens said, noting that this provided part of the rationale for testing an immunotherapy drug plus chemotherapy in patients.
"Adding chemotherapy to immunotherapy has been successful in other cancers,” she said. “The idea is that chemotherapy can break open cancer cells and release proteins that immune cells can then recognize and use to attack the tumor.”
The clinical trial was sponsored by the manufacturer of atezolizumab, Roche/Genentech.
A Difficult-to-Treat Disease
“This is a possible therapeutic option for patients with a subtype of breast cancer that is difficult to treat,” said Jung-Min Lee, M.D., in the Women’s Malignancies Branch of NCI’s Center for Cancer Research, who was not involved in the study.
“There are no specific targeted drugs for patients with triple-negative breast cancer, and recurrence is common,” Dr. Lee continued. “Once it recurs, the disease is very difficult to treat.”
The increase in median progression-free survival is a “meaningful” improvement for patients, said Dr. Lee, noting that the combination was well tolerated. “Patients want to have not only an improved quantity of life but also a good quality of life.”
The most common side effects in the atezolizumab group included hair loss, peripheral neuropathy, cough, fever, fatigue, neutropenia, and nausea. There was also more hypothyroidism in the atezolizumab group, but doctors could manage this side effect, Dr. Emens noted.
Dr. Lee cautioned, however, that even among the patients whose tumors expressed PD-L1, there were some who did not respond well to the atezolizumab–chemotherapy combination, including those patients with advanced disease that had spread to the liver, lung, or bone.
Future Research
“I’m excited about this new approach, but as clinicians, we have to use the combination therapy wisely,” Dr. Lee said.
Doctors need to consider the risks and benefits of using the combination to treat patients with advanced disease who have certain metastases, as well as patients who have mutations in the BRCA1 or BRCA2 gene, she continued.
Additional clinical trials are needed to inform future discussions between patients and physicians about using the combination treatment, Dr. Lee added.
“We also need to develop immunotherapy-based strategies for the group of patients whose tumors are not PD-L1–positive,” said Dr. Emens. Another goal for future research is to test immunotherapy-based treatments earlier in the course of the disease, she added.
No comments:
Post a Comment