
What Can We Learn from EEG’s of Patient’s with Epilepsy?
Skip to:
Epilepsy is a neurological condition characterised by recurrent episodes of seizures. Most cases of epilepsy do not have a clear cause. The primary pathogenesis of many forms of epilepsy is an abnormal expression of certain receptors in the brain that lead to enhanced excitation and reduced inhibition, leading to increased neural activity.

Girl with EEG electrodes attached to her head for medical test Credit: Vasara / Shutterstock
What is an EEG?
An EEG, or electroencephalogram, is a non-invasive diagnostic and research tool used to study a patients’ brains electrical activity (brain waves). During the procedure, small electrode sensors attached to sticky pads are attached to the scalp across the head which are sensitive to the electrical activity in the brain.
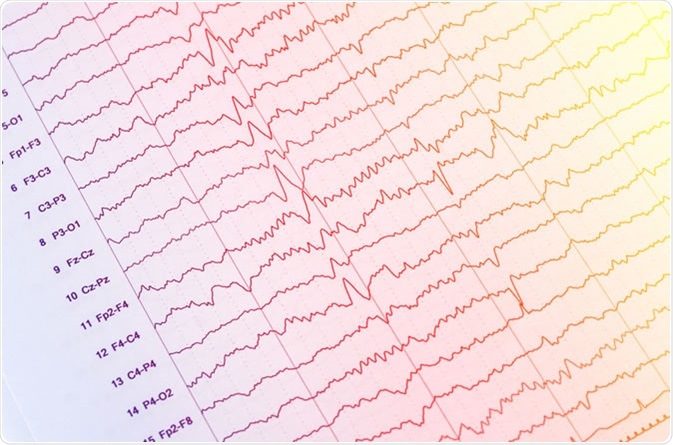
EEG - electroencephalogram output - Image Credit: Chaikom / Shutterstock
An EEG is typically carried out by a specialist clinical neurophysiologist or psychiatrists and can be done at the clinic or at home. Though EEG has many research uses across a variety of psychiatric and neurological conditions, in the clinic, it is typically almost exclusively used to diagnose and monitor epilepsy. Depending on the type of brain waves being produced, clinicians can identify a specific type of epilepsy and offer more tailored treatment strategies.
EEG and Epilepsy
Epilepsy is characterised by periods of intense electrical activity in the brain during a seizure. This is thought to be primarily due to increased excitation in the brain coupled to reduced inhibition, causing neurons to fire excessively. Interictal epileptiform discharges (IEDs) are characteristic waves which differentiate epileptic and nonepielptic attacks. These include spikes, sharp waves, spike-wave complexes and polsypikes in an EEG recording.
However, seizures only occur occasionally, and unless a seizure is occurring, an EEG will not pick up seizure-like activity (status epilepticus). Due to this, it is important that patients suspected of epilepsy are offered repeated EEGs on a long-term basis as this increases the diagnostic yield and chance of picking up IEDs. Sleep deprivation, hyperventilation and photic stimulation can enhance the likelihood of picking up epileptic EEG signals in over half of suspected patients. Other forms of epilepsy; especially in children, may happen during sleep, so a sleep EEG test may also be offered.
In certain forms of epilepsy, the brain remains highly excitable at rest, and an EEG may therefore be able to confirm diagnosis. Some specific examples are:
- Anterior temporal lobe spikes are a sign of mesial temporal lobe epilepsy
- Generalised 3 Hz spikes are indicative of absence epilepsy
- >4 Hz spikes & generalise polyspikes are characteristic of Lennox-Gastaut syndrome
- Extratemporal polyspikes are due to focal cortical dysplasia
Due to the similarities of ‘normal’ sharp waves and patterns, EEG patterns can be often misinterpreted even amongst specialists. For example, 7 Hz rhythmical temporal theta waves in the temporal cortex are often a sign of drowsiness in young adults, but may be confused with epilepsy. Other examples include a sporadic small sharp spike (50 ms) in the frontal lobe which are actually indicative of ‘benign epileptiform transients of sleep’ rather than IEDs. Most of the confusing signals arise due to relaxed or early sleep stages in adults.
Other EEG Techniques
EEG is typically a non-invasive technique with electrodes placed on the scalp. Typical EEG has evenly spaced electrodes over a large area of the head. Though this may provide useful information as to the neural electrical pattern and some level of localisation, it is not entirely spatially accurate. As such, there are two further EEG options that can provide even more in-depth information:
1) Dense Array EEG (daEEG). daEEG is EEG but with a higher number of surface electrodes at greater density and thus can cover a larger area of the skull enhancing spatial resolution. Using this new technique, researchers were able to identify that in most seizure types tested, a cortical slow-wave (CSW) appeared after the seizure, and the number of CSWs correlated with the severity of the seizure. This wave also spread from the temporal lobe (site of onset) towards the frontal lobe as well as to the other hemisphere. This study highlights that more sensitive electrical patterns can be picked up in the brain even when a seizure is not taking place that conventional EEG cannot observe.
2) Invasive EEG. Invasive EEG is typically only considered for patients undergoing surgery. Here, the electrodes are placed directly on the brain surface, or deep within a region of the brain. This allows spatially accurate localisation of the origin of the epilepsy. It can also be used for cortical mapping in which different tasks relate to different neural patterns in different parts of the brain, to ensure that things like memory and speech are not affected due to surgery. Invasive EEG has a much better signal to noise ratio
In summary, an EEG is the best diagnostic and research tool we have to study brain waves (neural patterns) in control subjects and patients with epilepsy. EEG can give information about the type of epilepsy as well as some level of localisation. Whilst not perfect, and prone to misinterpretation, EEG remains the gold-standard of epilepsy diagnosis. Newer EEG techniques allow for better localisation of epilepsy within the brain.
Sources
- Epilepsy Action (2019). epilepsy.org.uk https://www.epilepsy.org.uk/info/diagnosis/eeg-electroencephalogram
- Noachtar & Remi, 2009. The role of EEG in epilepsy: a critical review. Epilepsy Behav. 15(1):22-33. https://www.ncbi.nlm.nih.gov/pubmed/19248841
- Yang et al, 2012. Spectral and spatial shifts of post-ictal slow waves in temporal lobe seizures. Brain. 135(1):3134-43 https://www.ncbi.nlm.nih.gov/pubmed/22923634
Further Reading
Last Updated: Oct 24, 2019

No comments:
Post a Comment