Advances in Thyroid Cancer Research
NCI-funded researchers are working to advance our understanding of how to treat thyroid cancer. Most thyroid cancers are found at an early stage and can be treated successfully. Scientists are now working to understand which people with thyroid cancer can safely choose less treatment for their disease, to minimize side effects. Research is also needed to find new treatments for rarer, aggressive types of thyroid cancer.
This page highlights some of the latest research in thyroid cancer, including clinical advances that may soon translate into improved care, NCI-supported programs that are fueling progress, and research findings from recent studies.
Thyroid Cancer Diagnosis
Over the last two decades, a major concern regarding thyroid cancer has been overdiagnosis - that is, the detection of small, slow-growing thyroid tumors that may never cause a medical problem. These tumors, also called nodules, are detected through screening, either by feeling the neck or using ultrasound.
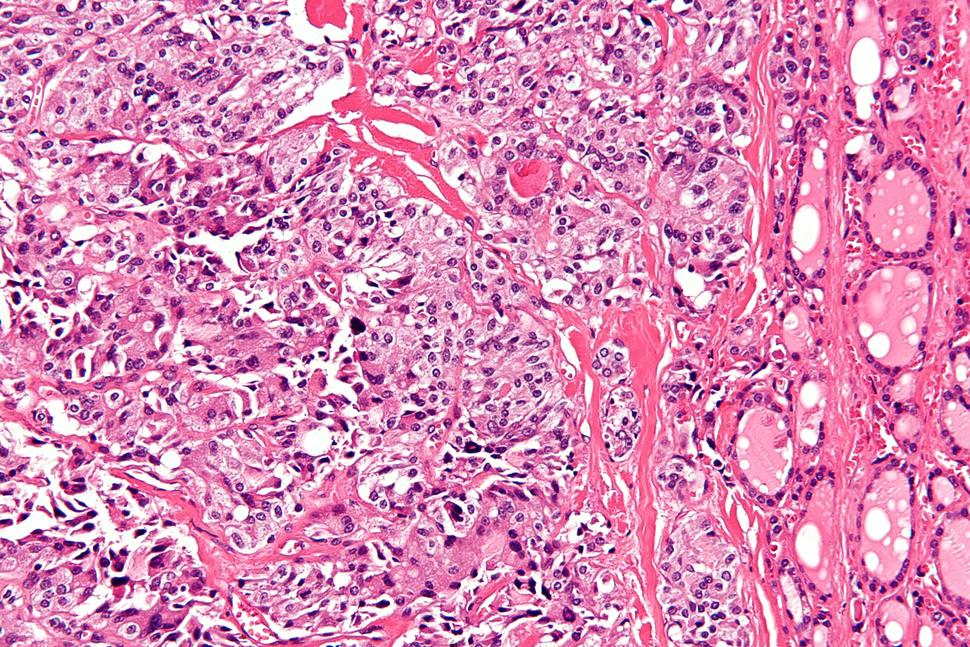
When a suspicious nodule is found on a person’s thyroid, a fine needle biopsy is often used to determine whether the mass is cancerous.
However, up to one-third of the time, pathologists can’t determine from the appearance of the cells whether a nodule is cancerous. In the past, people with inconclusive biopsy results would have had to undergo removal of the half of the thyroid (called a lobe) that contained the suspicious mass. In many cases, this turned out to be overtreatment because the mass did not contain cancer.
In the last several years, however, NCI-funded researchers have developed genomic tests that can help tell whether such inconclusive nodules are cancerous and require surgery. These tests have the potential to spare many people potentially unnecessary surgery. In the future, the tests may also be used to select treatments that match the genetic characteristics of individual cancers and determine how much of the thyroid to remove.
Papillary Thyroid Cancer Treatment
Most people diagnosed with thyroid cancer have a type called papillary thyroid cancer, which is slow growing and can usually be cured by surgery to remove the entire thyroid. Sometimes, if papillary thyroid cancer is more advanced, patients will also receive treatment with radioactive iodine.
Because the prognosis for early-stage papillary thyroid cancer is so good, scientists have been studying whether some patients can safely receive less extensive surgery. This would spare them the need to take thyroid replacement hormones for the rest of their lives. Treatment options could include:
- Having a lobectomy. A lobectomy is a type of surgery that removes half of the thyroid, leaving the other half in place to produce hormones. This type of surgery is already used for people with small papillary cancers. Recent findings suggest that some people with these cancers that are between 1 and 4 centimeters in size, and have not spread to the lymph nodes, may also opt for this surgery. Researchers are continuing to study whether more people with papillary thyroid cancer could choose to avoid surgery to remove the whole thyroid.
- Deferring surgery. Other research has shown that most people with very small papillary thyroid cancers—less than 1 centimeter—don’t need to have any type of surgery immediately. They can be safely monitored with periodic ultrasound imaging and have surgery only if their cancer starts to grow.
Aggressive papillary thyroid cancer
In rare cases, papillary thyroid cancer can be aggressive and progress despite surgery and radioactive iodine treatment. In recent years, the Food and Drug Administration (FDA) has approved two targeted drugs for such cancers: sorafenib tosylate (Nexavar) and lenvatinib (Lenvima). Both drugs block the action of several different altered proteins that promote cancer cell growth.
One of the altered proteins that sorafenib blocks is produced by a mutant form of the BRAF gene. This gene is found in some patients and promotes the development of aggressive papillary thyroid cancer. Additional drugs that target this altered B-Raf protein are being tested in people whose papillary thyroid cancer has recurred or progressed despite treatment.
NCI researchers are also studying how the B-Raf protein interacts with other proteins, with the goal of identifying new drugs that target these interactions. Additionally, researchers are looking for other genetic mutations in papillary thyroid cancer that could be targeted with new treatments.
Medullary Thyroid Cancer Treatment
A rare type of thyroid cancer called medullary thyroid cancer begins in the thyroid cells that produce a hormone called calcitonin. Radioactive iodine is not effective for these cancers, so targeted therapies may be used if the disease recurs after surgery or if it has spread elsewhere in the body (metastasized). NCI researchers are looking for better drugs for the treatment of medullary thyroid cancer:
- Scientists in NCI’s Surgical Oncology Program are collaborating with the National Center for Advancing Translational Sciences (NCATS) to screen thousands of potential drug candidates to see if they can kill medullary thyroid cancer cells. Any promising drugs will eventually be tested in clinical trials at the NIH Clinical Center.
- In 2018, NCI’s My Pediatric and Adult Rare Tumor (MyPART) network started a rare tumor clinic for people with medullary thyroid cancer that doesn’t respond to standard treatments or recurs after treatment. Researchers will use tissue samples collected from clinic participants to try and understand how these cancers differ genetically from those in which existing treatments are effective.
- Recent work from the NCI researchers in charge of the MyPART clinic showed that the drug vandetanib (Caprelsa) can safely slow tumor growth in children and adolescents with inherited syndromes that cause medullary thyroid cancer.
- Researchers have recently found that tiny deposits of medullary thyroid cancer cells can be seen on PET scans by using a radioactive tracer called gallium Ga 68-Dotatate, which binds to those cells.
Scientists are now interested in seeing if a related drug, called lutetium Lu 177-Dotatate (Lutathera), could be used as a treatment for medullary thyroid cancer. Lutetium Lu 177-Dotatate could potentially be used to deliver therapeutic radiation directly to medullary thyroid cancer cells. The drug is already approved for the treatment of some rare tumors of the digestive tract.
Anaplastic Thyroid Cancer Treatment
Anaplastic thyroid cancer is rare but it is the most aggressive type of thyroid cancer and one of the most aggressive cancer types overall. Historically, few people with this disease are still alive one year after diagnosis.
Until recently, no drugs were approved for the treatment of anaplastic thyroid cancer because the disease had proved resistant to all tested therapies. But in 2018, FDA approved the combination of two targeted drugs, dabrafenib mesylate (Tafinlar) and trametinib (Mekinist), for anaplastic thyroid cancers that have a certain mutation in the BRAF gene. About a quarter of anaplastic thyroid cancers carry this mutation.
Researchers at NCI and elsewhere are now looking for additional mutations in anaplastic thyroid cancer that could be targeted with existing drugs. Through the collaboration between NCI’s Surgical Oncology Program and NCATS, researchers are screening drugs approved for other conditions for the potential use of treating anaplastic thyroid cancer.
NCI-Supported Research Programs
See a full list of thyroid cancer research projects that NCI funded in FY 2017.
The Thyroid Specialized Programs of Research Excellence (Thyroid SPOREs) are designed to quickly move basic scientific findings into clinical settings. The Thyroid SPOREs support the development of new therapies and technologies, as well as studies to better understand the genetics, biomarkers, and treatment of thyroid cancer.
Scientists in NCI's Division of Cancer Epidemiology and Genetics (DCEG) conduct both national and international research on thyroid cancer. Studies include those that have an environmental focus, such as exposure to radiation and thyroid cancer, as well as those analyzing physical risk factors and thyroid cancer.
Clinical Trials
NCI funds and oversees both early- and late-phase clinical trials to develop new treatments and improve patient care. Trials are available for thyroid cancer treatment.
Thyroid Cancer Research Results
The following are some of our latest news articles on thyroid cancer research:
- Genomic Test Helps Identify Thyroid Nodules That Don’t Require Surgery
- Dabrafenib–Trametinib Combination Approved for Melanoma, Anaplastic Thyroid Cancer
- Patients Who Choose No Intervention for Small Thyroid Cancers Report Lack of Support
- After Rising for Decades, Thyroid Cancer Incidence Stabilizes
- FDA Approves Lenvatinib for Radioactive Iodine-Refractory Thyroid Cancer
- TCGA Study Improves Understanding of Genetic Drivers of Thyroid Cancer
View the full list of Thyroid Cancer Research Results and Study Updates.
No comments:
Post a Comment