
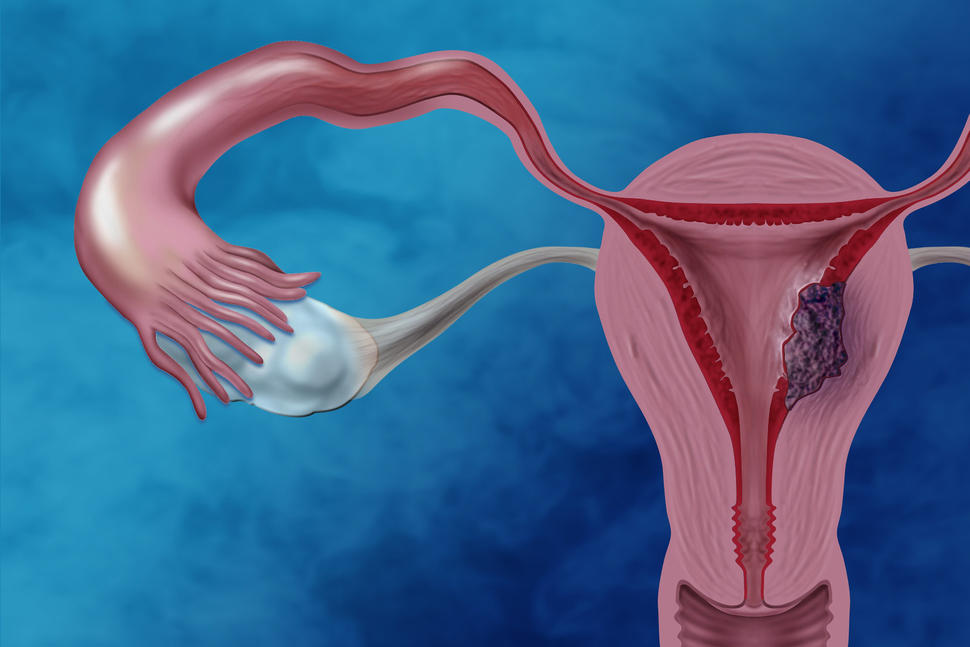
Can Some Women Treated for Endometrial Cancer Forgo Radiation after Surgery?
, by NCI Staff
Some women with endometrial cancer may be able to receive less intensive treatment than is commonly given to patients without increasing the risk of the disease recurring within 5 years, according to the results of a randomized clinical trial.
In the NCI-funded study, women with locally advanced endometrial cancer who received chemotherapy after surgery were no less likely than women who received chemotherapy plus radiation (chemoradiation) after surgery to have a recurrenceof their cancers in 5 years.
The trial included more than 700 women who initially had surgery to remove endometrial cancer, the more common type of uterine cancer. Participants were randomly assigned to receive either chemoradiation or chemotherapy alone. The median follow-up period was 47 months.
Five years after starting treatment, the rates of recurrence-free survival were estimated to be similar between the groups: 59% among women who received chemoradiation, and 58% among women who received chemotherapy alone. The results were published in the New England Journal of Medicine on June 13.
“The bottom line is that chemotherapy alone was as good as chemotherapy with radiation therapy in terms of recurrence-free survival,” said David Mutch, M.D., of the Washington University School of Medicine in St. Louis and an investigator on the trial.
The results of the study “tell us at a broad level that either treatment approach is reasonable,” said Elise Kohn, M.D., head of Gynecologic Cancer Therapeutics in NCI’s Division of Cancer Treatment and Diagnosis, who was not involved in the study.
But she noted that the study also revealed subtle differences in patterns of recurrences between the treatment groups that could help physicians to develop more individualized treatment regimens for women with endometrial cancer.
For example, patients who are at an increased risk of a recurrence in the pelvic area may be candidates to receive the combination of chemotherapy and radiation therapy, Dr. Kohn said.
Treating Locally Advanced Endometrial Cancer
Most cases of endometrial cancer are diagnosed at an early stage and can be cured with surgery. Patients with locally advanced disease (that is, stage III or IVA) have cancer that has spread outside the uterus but has not invaded other organs, such as the lungs or liver.
“We focused on this group because these women are at risk for the disease recurring in the pelvic region and also in other parts of the body,” said Daniela Matei, M.D., of Northwestern University Medical School, who led the study.
Radiation to the pelvic region or whole abdomen in women with locally advanced endometrial cancer who have received surgery can reduce the risk of the disease returning in those areas. But radiation is less effective than chemotherapy at reducing the risk of recurrences elsewhere in the body.
Researchers have hypothesized that combining chemotherapy and radiation would help prevent recurrences both in the pelvic region and in other parts of the body, and indeed many women receive chemoradiation after surgery. But until now there had not been a large randomized phase 3 trial comparing the two approaches in women with locally advanced endometrial cancer.
“This clinical trial was designed to answer the question of whether chemoradiation was superior to chemotherapy alone,” said Dr. Matei, noting that she had expected the study results to favor chemoradiation.
Results of the Study
To compare the treatment approaches, Dr. Matei and her colleagues recruited 736 women with locally advanced endometrial cancer in the United States and other countries.
Although women in the chemoradiation group were less likely to have recurrences in the pelvic region than women in the chemotherapy group, they were more likely to have tumors in areas outside the pelvic region, the researchers found.
Specifically, the combined-treatment group had a lower 5-year incidence than the chemotherapy group of vaginal recurrence (2% versus 7%) and of pelvic and nearby lymph-node recurrence (11% versus 20%). But the chemoradiation group also had a higher incidence of recurrence in other parts of the body (27% versus 21%).
In general, patients tolerated both treatment regimens similarly, the researchers found. There were also no major differences in the quality-of-life scores between the treatment groups, according to surveys of participants, Dr. Kohn noted.
Although acute side effects were more common in the combined-treatment group than in the chemotherapy-alone group, most were low grade and reversible when treatment was discontinued, the study authors noted.
“Chronic toxic effects included diarrhea, lymphedema, and musculoskeletal events and were more common with chemoradiotherapy,” they wrote.
The cumulative effects of radiation therapy can lead to irritation of the lower gastrointestinal tract, which may result in diarrhea, explained Dr. Kohn. There may also be some risk of scar tissue developing, depending on the type of radiation therapy a patient receives.
For some patients, traveling to a treatment facility every day to receive radiation therapy might be a significant burden, she continued. This consideration could be part of discussions between doctors and patients about possible treatments, Dr. Kohn added.
Finding the Optimal Treatment for Patients
Dr. Matei said that the study results, which have been presented at scientific meetings, are already a matter of debate among oncologists.
“Some institutions have embraced the results of the trial and have fundamentally changed their approach to treatment of locally advanced endometrial cancer by focusing on chemotherapy alone,” Dr. Matei said.
Other physicians, she noted, are “putting more weight on the combined approach and believe that the local control offered by radiation, which was clearly demonstrated in the trial, is worth the additional cost and increased risk of chronic toxicity.”
Still other physicians, Dr. Matei went on, “favor a personalized approach” that considers a patient’s estimated risks of relapse in the pelvic region and other parts of the body.
More research is needed, Dr. Mutch said, to determine the optimal treatment for patients with locally advanced endometrial cancer.
“We need to understand the molecular differences in the tumors of patients with endometrial cancer and, if possible, try to target the specific abnormalities in these tumors,” he added.
No comments:
Post a Comment